News
Early Detection Saves Lives: Start with a Self-Exam

When is your next period? This time around, consider giving yourself a self-breast exam one week after your period ends. Breasts tend to be less tender and swollen at this time, making it easier to feel for any potential changes or lumps. While self-breast exams are not the main form of screening, they are still an important tool for empowering women to take control of their personal health and wellness.
Becoming familiar with your own breast tissue will allow you to increase your ability to notice any changes. Following is an easy six-step process for doing a breast self-exam, as well as some tips from Samantha DelNegro, PA, and Stephanie A. Miller, MD, MBA on what to look for.
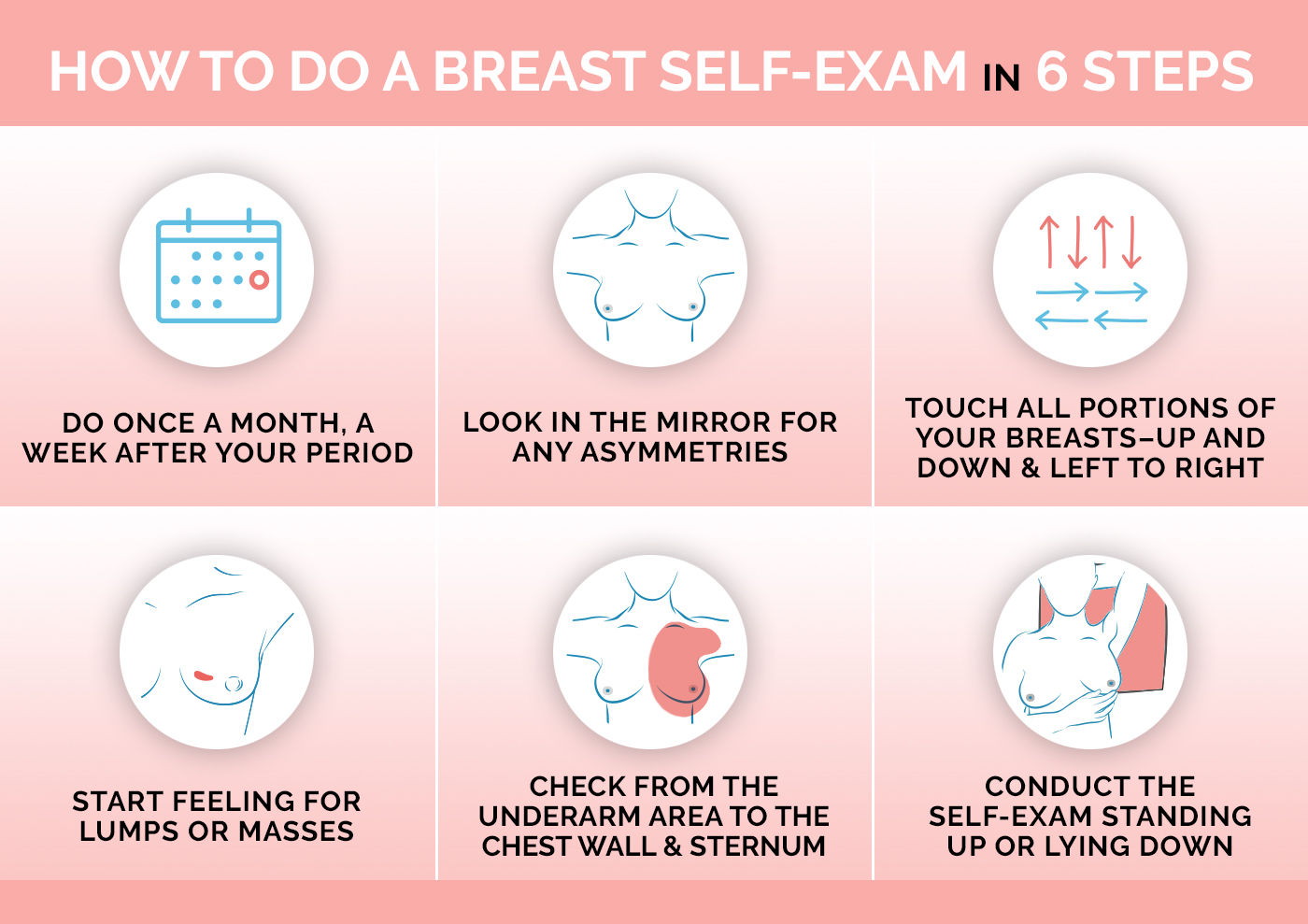
Images courtesy of Samantha DelNegro.
What to Do if You Detect a Lump in Your Breast
Finding a lump in your breast can be concerning, but it's important to remember that over 90% of lumps are non-cancerous and may result from normal changes in the breast tissue. That said, it’s always important to take the right steps to evaluate and address any changes in your body. If you feel a change in your breast, take the following steps.- Schedule an appointment with your primary care provider or OB/GYN
- If you do not have a primary care provider or OB/GYN, call Colorado Mountain Medical or Mountain Family Health to find one.
- Jot down some notes
- Write down when you first noticed the lump and any other related symptoms to share with your healthcare provider. Draw a diagram on a piece of paper, noting details of the lump, and keeping track of any changes after each self-exam.
- Gently feel the lump and try to determine its size, shape, and whether it’s hard or soft.
- Take note of the location of the lump in the breast.
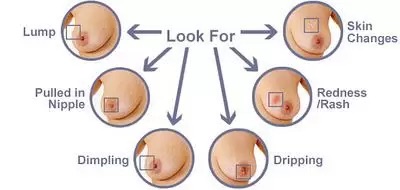
- Pay attention to any changes in the skin of your breast (such as redness or dimpling), changes in nipple appearance, or unexplained pain.
- Consult with your primary care provider or OB/GYN
- Your provider will perform a clinical breast exam to assess the lump and your overall breast health and will work with you to determine next best steps.
- Be open about your concerns. During the appointment, make sure to mention any family history of breast cancer, personal breast history or other relevant health issues, as this information will help guide further evaluation.
- Diagnostic imaging
- If your healthcare provider believes the lump requires further investigation, you will be recommended for diagnostic imaging, such as:
- Mammogram: A breast X-ray that can provide detailed images to help assess the lump.
- Ultrasound: A non-invasive imaging technique that uses sound waves to create an image of the breast tissue. Ultrasound is often used to distinguish between a solid lump and a fluid-filled cyst.
- MRI: In certain cases, an MRI may be recommended for a more detailed view.
- If your healthcare provider believes the lump requires further investigation, you will be recommended for diagnostic imaging, such as:
- Biopsy (if needed)
- If the diagnostic imaging tests raise concerns, or if the lump remains suspicious, your provider may recommend a biopsy. This involves taking a small sample of the tissue from the lump to examine it under a microscope for signs of cancer or other conditions.
- A biopsy can often be done using a core needle, which is minimally invasive.
- Follow-Up Care
- Once the evaluation is complete, your provider will discuss the results with you and explain the next steps based on the findings. If the lump is benign, you may be recommended for routine monitoring or a follow-up exam in a few months.
- If the lump is found to be cancerous or pre-cancerous, your healthcare provider will guide you through treatment options and initiate the appropriate referrals.
- Women with an average risk of breast cancer are recommended for annual screening mammograms starting at age 40.
- Women with higher-than-average risk of breast cancer may need earlier and more frequent screening with mammography in addition to imaging options such as breast ultrasound, and possibly MRI.
- Women with dense breasts (50% of women in the U.S.) may be offered supplemental screening in addition to mammography due to increased risk of a false negative mammogram result.
